The matchup: Two doses of psilocybin, the active ingredient in “magic mushrooms,” against a six-week course of the popular antidepressant escitalopram, often sold as Lexapro or Cipralex. Escitalopram is one of a class of antidepressants called selective serotonin reuptake inhibitors, or SSRIs.
The projected winner: The drug that produces the best outcome at six months in the battle against depression, which affects more than 300 million people worldwide.
The stakes are high for psilocybin clinical trials — there’s a pressing need for a more effective medical solution in the fight against depression, especially treatment-resistant depression. Of the nearly 9 million people with major depression in the United States who have tried pharmaceuticals, 2.8 million are estimated to be resistant to multiple antidepressants.
“I am aware of a case of a person who tried 17 different drugs and nothing worked,” said psychobiologist Dr. Bertha Madras, director of the Laboratory of Addiction Neurobiology at Harvard Medical School’s McLean Hospital in Belmont, Massachusetts.
“Even shock therapy failed,” Madras said. “It’s a terrible thing when you simply cannot help a person to get up out of bed and engage in life.”
Antidepressant pros and cons
For a good number of people antidepressants have been a blessing, at least at the beginning of treatment, said Dr. Charles Raison, a professor of psychiatry and human ecology at the University of Wisconsin School of Medicine and Public Health in Madison.
“I always start by saying, ‘Thank God, we have them.’ Many people can say, ‘Wow, I was pulled out of a pretty deep hole,’“ said Raison, who is also the director of the Vail Health Behavioral Health Innovation Center in Colorado where psilocybin is studied.
But for up to a third of depressed patients, antidepressants fail to work at all. Even for those who do find relief, “the benefits tend to fade in some fairly reasonable percentage of people over time,” Raison added. “Then there’s the side effects, many of which don’t get much better long term.”
Initial reactions such as nausea or headaches often fade within a few weeks after starting an antidepressant, but sexual side effects such as reduced libido and difficulty with orgasm can last for months or even years. In rare cases, sexual dysfunction can persist even after stopping the antidepressant.
That’s one problem that psilocybin doesn’t have, said psychedelics researcher David Nutt, director of the neuropsychopharmacology unit at Imperial College London’s division of brain sciences.
“If you have just one trip and get better, there’s no drug in you day after day and no long-term sexual side effects,” Nutt said.
Psilocybin also has the edge when it comes to emotional blunting, which is the tendency of antidepressants to diminish not only depression but also enjoyment in life.
“This is such a consistent finding in studies, it’s become the theory of how antidepressants work — they suppress the brain’s supersensitive stress center and allow it to heal,” Nutt said.
“However, the pleasure center of the brain can also be dampened, and we know that because when we put people on antidepressants in the brain scanner, they don’t respond as much as to happy faces,” he added.
“Some people don’t like that. They say, ‘I don’t enjoy life as much. I’m not depressed anymore, but I’m not as happy.’”
The top psychedelic contender
In the search for a new alternative in treatment, psilocybin entered the ring as a fan favorite — arguably the most popular of a lineup of psychedelic drugs that last saw their heyday in the Timothy Leary era of the 1960s.
In small clinical trials, synthetic versions of the psychedelic have shown benefits in tackling cluster headaches, anxiety, anorexia, obsessive-compulsive disorder and various forms of substance abuse.
Still, psilocybin’s highest accolades have come from the drug’s apparent success in treating depression. Three versions of synthetic psilocybin have received the US Food and Drug Administration’s “breakthrough therapy” designation — in 2018 for treatment-resistant depression, which is diagnosed when people have tried and failed multiple antidepressants — and in 2019 and 2024 for clinical depression, diagnosed when a person is severely depressed most of the time.
Breakthrough status is a designation that can fast-track the road to FDA approval and is given to drugs that “demonstrate substantial improvement over available therapy,” according to the agency.
Another key contender, MDMA, or 3,4-Methylenedioxymethamphetamine, commonly known as Molly or Ecstasy, shows promise in treating post-traumatic stress disorder, or PTSD, but hasn’t been directly studied for depression.
In 2024, lysergic acid diethylamide, better known as LSD, won FDA breakthrough status for treating anxiety. It’s also in clinical trials for depression. Smaller clinical trials for less well-known psychedelics are also underway.
Not everyone in the field is convinced that psilocybin — or any other psychedelic — will survive FDA scrutiny. In August, the agency surprised researchers by rejecting MDMA as a treatment for PTSD, sending its maker back to conduct another clinical trial that could take years.
“We have no idea how these drugs will fare in a much larger population of people,” said Harvard’s Madras.
“To say that psilocybin is going to be the magic bullet that will solve the problems of depression, I think, is irresponsible at best and hazardous at worst.”
A more open brain
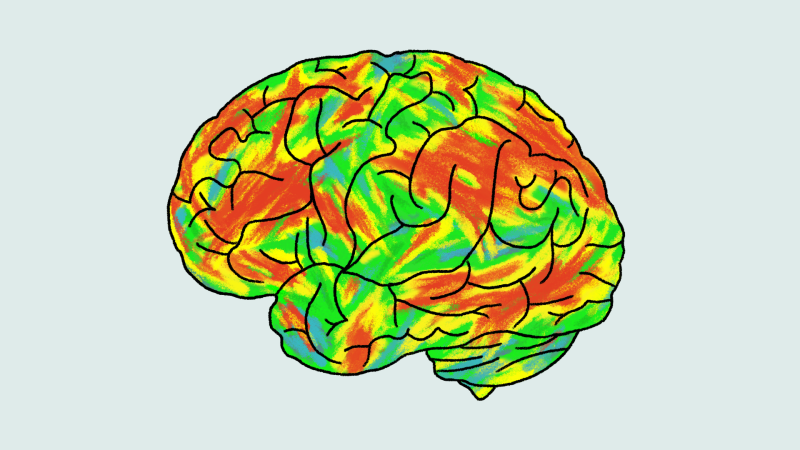
Psilocybin works on a different part of the brain than antidepressants, expert says. The psychedelic zeros in on the brain’s ruminative area, where thoughts run in a circular wheel of negativity many find hard to stop. Brain scans taken before, during and after people are tripping on psilocybin show the brain becomes desynchronized —disrupting those negative thoughts and allowing people to see themselves differently.
“People begin to feel, understand and appreciate that their brain can change and they can escape from their depression,” Nutt said. “They can look through a door to a different way of thinking, and they can then walk through the door afterwards.”
Integrating those new insights into daily behavior that lasts, however, is the key to long-term success in fighting depression, experts say. That’s why studies on psilocybin have used trained therapists during the hallucinogenic trip, along with therapy sessions before and after the experience.
“The psychedelic experience opens up this sort of critical period where your brain is more open, sprouting new brain cells, somewhat like a child’s brain,” Raison said.
“But what if you get in a car wreck or your husband leaves you the next day? What if it alters your mental status in ways that make you want to fly so you jump off a bridge? It doesn’t happen often, but that’s the risk.”
Psychedelic therapists sometimes do report adverse outcomes, such as difficulty adapting to life post-treatment and a worsening of anxiety and ruminative brooding, the very conditions psychedelics are supposed to help. Even if such reactions are rare, Raison said, they point to the larger problem of prescribing psilocybin — or any other psychedelic — to the general population.
“Let’s say only 2% or 3% of people get really screwed up after a trip,” he said. “If you have 20 million people doing a trip, it’s a problem. These agents are really powerful.”
Promising but inconclusive results
The original April 2021 study pitting psilocybin against escitalopram was a double-blinded, randomized controlled trial of 59 patients with either moderate or severe depression. Thirty patients were treated with two 25-milligram doses of psilocybin administered three weeks apart, while the other 29 received one tiny 1-milligram dose of psilocybin along with a six-week course of escitalopram. Both groups received about 20 hours of psychotherapy.
“This is the first time anyone has looked at the longer-term behavioral effects of psilocybin compared to something else — and probably the only time anyone will ever do a long-term comparison of psilocybin to an SSRI,” said Raison, who was not involved in the study. “For that reason alone, this research matters.”
At six weeks, the study found no significant difference in depression scores between the antidepressant and psilocybin groups. Brain scans, however, showed a different story.
“The brains of people on psilocybin had increased flexibility, a greater ability to switch between different brain states,” said Nutt, who was a coauthor on the study.
Nutt and his team published the six-month results of the same group of patients in September. While both psilocybin and escitalopram showed comparable improvement in depressive symptoms, people who took psilocybin reported greater joy in their lives — a significant plus in keeping depression at bay.
“Psilocybin outperformed escitalopram in several measures of well-being — meaning in life, work and social functioning,” said lead researcher Tommaso Barba, a doctoral candidate at Imperial College London in a statement.
However, critics pointed out that people in the psilocybin arm of the trial were allowed to seek out additional therapy and even start antidepressants between the administration of psilocybin and the six-month check-in — behaviors that could have also contributed to improvement.
Regardless, the study found people who responded best to psilocybin on brain scans at six weeks reported the lowest levels of depression at six months, Nutt said.
“The more flexible a patient’s brain was three weeks after one trip, the better their outcome on depression at six months,” Nutt said. “There’s a biological, physiological change in the brain as a result of psilocybin — which you can see at three weeks after a trip — that predicts clinical outcome.
“But before we say it’s a fact, it needs to be replicated,” Nutt added.
Challenges for the future
Harvard’s Madras and other critics said a good deal about psilocybin and other psychedelics must be sorted before any could ever become a new treatment option for mental health.
“For one, clinical trials have focused on a restricted population. In some of the studies, 1,000 people are interviewed, and 50 are selected,” said Madras, who wasn’t involved in the escitalopram study.
“Why? Because they have to screen out people who might be susceptible to a psychotic break — anyone with family history of suicide, psychosis or bipolar disorder,” she said.
In fact, Madras said, adverse effects are such a concern that researchers in psychedelic clinical trials often actively recruit people who have successfully taken psychedelics in the past.
Then there’s the issue of blinding. In gold standard randomized clinical trials, patients are not supposed to know if they received a drug or a placebo, a fake pill designed to mimic the active ingredient in the treatment being tested.
If a drug is significantly more helpful than the placebo, that’s a good indication the positive effect isn’t due to a patient’s expectation of getting better and the clinical trial is a success.
However, finding a placebo that fools people into thinking they are on a hallucinogenic trip has proven challenging. In a study using psilocybin for alcohol substance abuse, for example, some 95% of those involved correctly guessed whether they were taking psilocybin or the placebo.
Then there’s the issue of cost. It’s yet to be determined if the intense therapy needed to bolster success with a psychedelic drug such as psilocybin will be affordable to the many depressed people who need it, Raison said.
“That’s the $1,000 question: How will this be brought to scale, and who will pay for it?” he said. “What’s it going to take for insurance to cover a treatment that’s administered say, two to three times a year that might cost $15,000 versus generic Prozac (fluoxetine), which costs five bucks a month?
“It is clear psychedelics work and have protracted benefits that we don’t yet understand,” Raison added. “But how that’s going to translate into long-term effectiveness against depression and how the health care system might deliver these at scale is still unknown.”